Welcome to the Aphasia Threads Project, which weaves together three points-of-view: people with aphasia, caregivers, and the professionals who help each family navigate aphasia. Each week, we bring together three unrelated stories, one from each member of this triad, to learn from their experience. This week, we’ll hear from Barbara, a person with aphasia after a stroke. Then, we’ll hear from Laura, who is a caregiver for her husband who has primary progressive aphasia. Finally, we’ll hear from Emily, a music therapist.

Person with Aphasia
A stroke. For about 6 days there was nothing going on. In the beginning, there was yes/no, a little something. It was all inside. I thought I was gonna die. If it’s the last thing I do, I will get better about it.
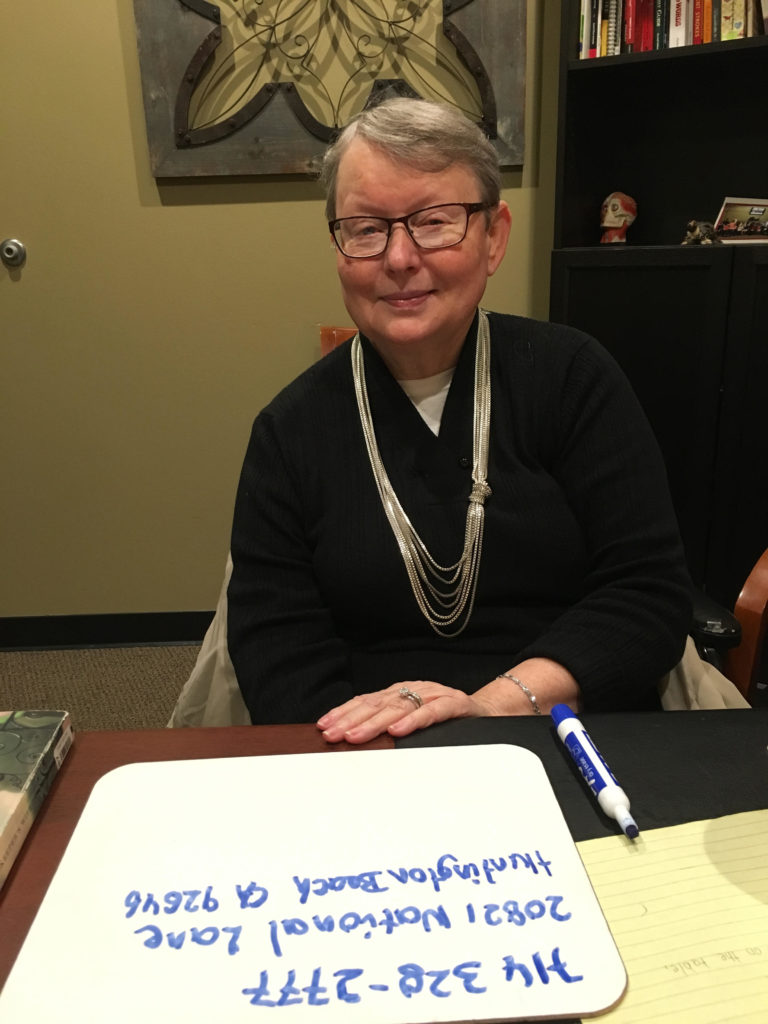
Aphasia Changes Your Life
I am a lot better. After 6 years, I am a lot better. I still don’t have it all back. My foot, arm, and speech (pointed to each area), it is all together. Well, I am very quiet and always was to a degree. I let him (husband) go (talk) the moment he says something that is not okay, I will tell him: “That’s it, no more, I am gonna take it!” Relationships: that is okay. I never even thought about it.
But There Are Things That Help
Everything is better because actually everything (all the therapies together) make it better. Everyday I have something (therapy: OT, PT, acupuncture, massage and speech). In the long run, it is all together.
And Things You Learn Along the Way
DON’T give up. DONT give up. Even if it’s just a little something. Even that first year, I had to work on everything, everything.
What Caregivers and Professionals Can Learn From Me
Always do and do it right. Do it right and see that we will get it better. It is better. It will get better. A little bit at a time. I am gonna get it right even if it kills me. I am gonna get it right.

Caregiver
My husband of 32 years was diagnosed with Primary Progressive Aphasia in 2011.

Aphasia Changes Your Life
Up until about 6 months ago, I was able to complete Roy’s sentences. I could figure out what he was wanting. Now it is extremely difficult, and I find myself telling him, “I’m sorry, I have no clue what you are saying” or “show me.” He can take me to whatever it is and then I understand. He has started using generic terms such as “it,” “that,” and “he/she.” He knows what “it” is, but he can’t say the word.
But There Are Things That Help
Roy was never computer savvy. I have downloaded the “Small Talk” apps, but he doesn’t understand how to use the device.
And Things You Learn Along the Way
Go to speech therapy, get online and research, and, most of all, be patient with the patient as they struggle. It is more difficult for them.
What People with Aphasia and Professionals Can Learn From Me
Caregivers and family are with this person daily, hourly, and every minute. It is important caregivers are patient. It is more important caregivers know the medical professionals have the ability to help. If the medical professional does not really understand the disease, if he/she is just going by book knowledge, it is extremely frustrating for the patient/family/caregiver. Please find us help, don’t just see us in your office for 15 minutes and send us away. Speech therapists have tried to work with Roy and have given him “homework” that he just cannot due anymore. He has lost the ability to read and write; therefore, help is very hard to find. We have given up on the medical community and work things out at home the best we can. I am a paramedic so I understand more than some, but I would love to find a speech therapist or neurologist that has experience with Primary Progressive Aphasia as well as Posterior Cortical Atrophy.
Roy is still Roy. He says people don’t want to talk to him anymore. He is embarrassed to try to have a conversation. When he does try, people stare and become uncomfortable. I usually have to finish the conversation for him. I have noticed that there are many people we used to talk to that avoid eye contact. I could care less, but I don’t want him hurt. He still wants to be part of conversations, and I try to keep him involved. Be patient with others. Be patient.

Professional
Emily works as a music therapist.
A client sought out music therapy to help with speech through singing.
What I’ve Noticed Along the Way
Joy — Seeing how music helps to transition from singing the word or phrase to speaking the word or phrase and how proud clients are of themselves when that happens. Frustration — When a client is trying to express themselves, and it’s difficult to even guess what they mean depending on their level of aphasia.
There Are Things That Help
Music therapy!
And I Encourage New Professionals to Learn About Aphasia
Patience is key; also gauging what is a good balance between challenging the client without making it too hard for him/her.
What People with Aphasia and Caregivers Can Learn From Me
Aphasia is always a work in progress. Even if a client can’t completely master a word or letter sound, it will inevitably come up again. Music therapy is so effective as it acts like a detour, routing to the other side of the brain around the affected area.

Want to Be Featured in a Future Article?
Aphasia Threads is an on-going project created by the National Aphasia Association. If you’d like to be featured, don’t leave a comment. Instead, please read the opening post for more information or fill out our form and we’ll contact you.



